![]()
Connect To Care FAQs
About Us

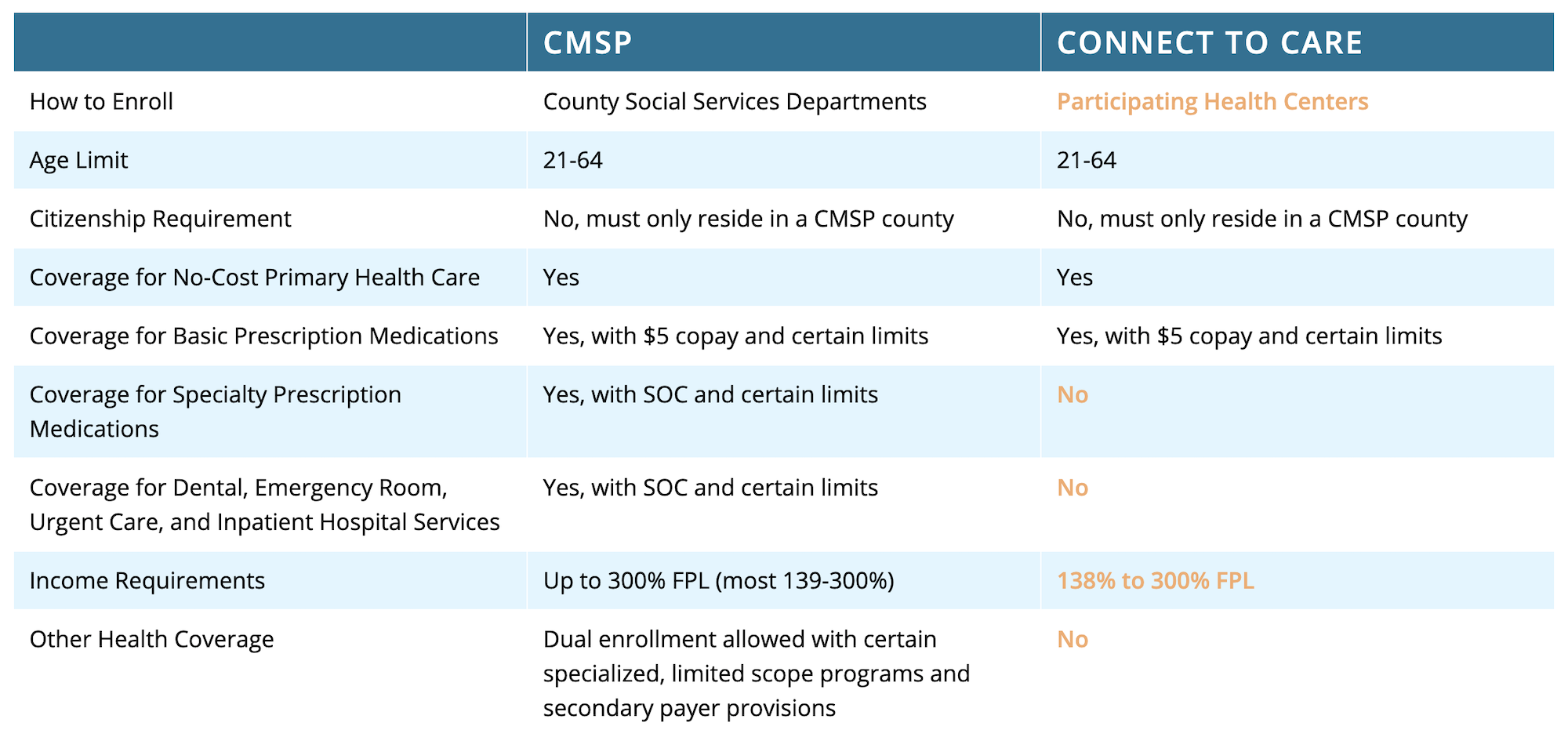
On December 1, 2020, the County Medical Services Program (CMSP) Governing Board launched the new Connect to Care Program. CMSP’s Connect to Care Program provides an alternate enrollment process at participating health centers for county residents to get coverage for CMSP-covered primary care services and prescription medications.
FREQUENTLY ASKED QUESTIONS
How do I qualify for connect to care?
To qualify for benefits, applicants must meet the following criteria:
- Ages 21 to 64 years old
- Live in one of the following counties: Alpine, Amador, Butte, Calaveras, Colusa, Del Norte, El Dorado, Glenn, Humboldt, Imperial, Inyo, Kings, Lake, Lassen, Madera, Marin, Mariposa, Mendocino, Modoc, Mono, Napa, Nevada, Plumas, San Benito, Shasta, Sierra, Siskiyou, Solano, Sonoma, Sutter, Tehama, Trinity, Tuolumne, Yolo and Yuba
- Have income between 138 percent –300 percent of the Federal Poverty Level. Learn more about the Federal Poverty Level here
- Be documented or undocumented
- Have no more than $20,000 in assets for a single person and no more than $30,000 in assets for a 2-person family
- Not currently enrolled in Medi-Cal, Medicare or have private health insurance
How do I sign up for connect to care?
- Find a Participating Provider
- Complete an application at a participating health center and bring the required documents
- After your application has been completed and accepted, you will receive an ID card and member guide in the mail within 10 days
How will my doctor or the pharmacy know that I’m enrolled in connect to care?
You’ll receive a Connect to Care ID Card (which will include the start and end dates of your coverage), a Connect to Care Member Guide, and Notice of Privacy Practices in the mail within 10 days of enrollment. If you need to fill a prescription before you receive your card, the pharmacy can look up your Connect to Care coverage with MedImpact by using your Connect to Care ID number or by calling (800) 788-2949. If you need to see a health care provider before you receive your card, AMM can verify your coverage by calling (888) 614-0846.
How do I get primary care services?
You can receive Connect to Care covered services at the health center where you completed your application, as well as other providers participating in the CMSP Provider Network. Covered benefits include:
- Screening for depression, alcohol misuse, obesity counseling (performed by a physician)
- Screenings for HIV, HPV, Hepatitis B & C, STI Screenings
- Various in-office minor medical procedures
- Outpatient mental health (mild to moderate) services
- Outpatient substance use disorder treatment services
- Physical Therapy
- Tobacco-use counseling and intervention (performed by a physician)
- Primary care or specialist office visits
- Preventative health screenings
- Routine screening laboratory testing
- Adult immunizations
- Specified X-rays of head, neck, chest, trunk, upper and lower extremities
- Specified ultrasound of head, neck, trunk, upper and lower extremities
- Colorectal cancer screening
- EKG, Osteoporosis, DEXA Scan
- Prescription medications with a $5 copay per prescription ($1500 maximum benefit limit)
The following services are not covered by Connect to Care:
- Emergency services (contact your County Social Services department to apply for the CMSP program)
- Inpatient hospital services (contact your County Social Services department to apply for the CMSP program)
- Pregnancy-related care (contact your County Social Services department if you become pregnant and need health care coverage)
- Dental care (contact your County Social Services department to apply for the CMSP program)
- Chiropractic or acupuncture care
- Out-of-network care
- Any procedure or service not included on the list of covered benefits
Connect to Care is the “payer of last resort” and is the secondary payer to state and federal health coverage programs. If you have HIV or AIDS, need family planning or infertility services, have Hepatitis C, or have breast or cervical cancer, you are required to seek eligibility with the following programs:
- California AIDS Drug Assistance Program (ADAP) for HIV and AIDS medications (call 1-844-421-7050)
- Family Planning, Access, Care and Treatment (Family PACT) for family planning and infertility treatment (call 1-916-650-0414)
- Medicine Assistance Tool (MAT) (visit https://www.medicineassistancetool.org)
- Breast and Cervical Cancer Treatment Program (BCCTP) (call 1-800-824-0088)
How do I fill my prescriptions at the pharmacy?
You need to go to a pharmacy contracted with Connect to Care/CMSP and show them your Connect to Care ID card. For a list of participating pharmacies, click here. Certain medications are covered by Connect to Care for a $5 per prescription co-payment. Connect to Care will pay for a maximum of $500 per prescription and up to $1500 for each enrollment period (6 months). For a list of medications covered by Connect to Care, click here.
How long does my connect to care coverage last?
After you complete your enrollment, your Connect to Care coverage will last up to 6 months starting from the day your application is submitted. Your Connect to Care ID Card will include the start and end dates of your coverage.
How do I re-apply for connect to care?
The reapplication process is the same as the application process. You may reapply at least 30 days prior to the end of your benefit period to avoid a gap in coverage. Please visit a participating health center to start an application for a new benefit period.